Fostering the Zone of Collaboration through Precision Radiology
Marcel Nienhuis
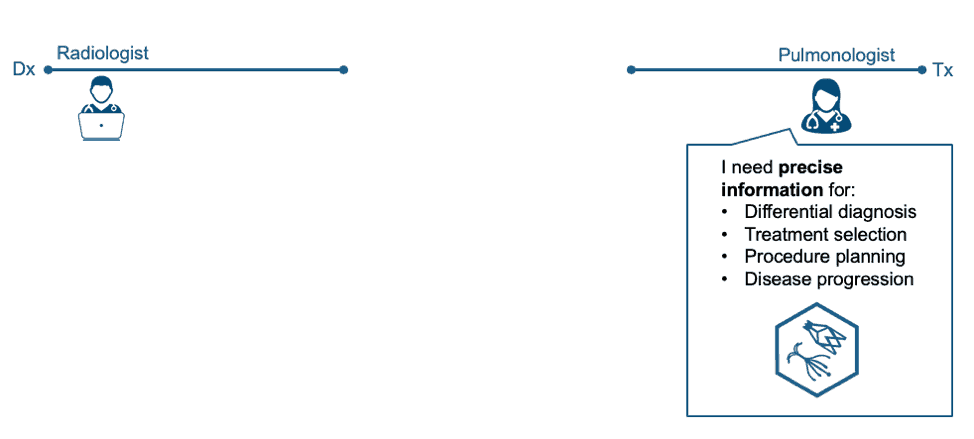
Pulmonology Clinician Needs
When speaking with clinicians (e.g. pulmonologists), we often ask “what kind of relationship do you have with your radiology department?” The most common answer goes something like this: “It’s OK. They give me a general report that provides some help, but I wish I could get more information.” Clinicians express a desire for precise imaging data to meet the needs of treatment decisions for modern therapies. For example, ELVR therapies are decided in part by collateral ventilation, which can be identified through fissure integrity. So, at one end of the hospital, we have clinicians craving more from their radiology departments.
Radiology’s Call for Change
Meanwhile, radiologists are aspiring to provide additional value. Radiology leaders have been increasingly urging their field to reinvent itself. Commonly heard messages include a desire to be more consultative, more collaborative, and patient-centric.
Here’s a sampling of recent quotes on this topic from thought-leaders in radiology:
- 2014: “We need to become better doctors—real doctors, if you will—who provide real value to our patients, our referring doctors and our hospitals," -David C. Levin, MD
- 2016: “We believe that radiologists should function not as production line workers, according to a factory model, but as consultants.” - Richard B. Gunderman, MD, PhD and colleagues.
- 2016: “We too must be on speed dial with our referring clinicians…we must offer customized and specialized imaging that will enhance our referring clinicians’ ability to deliver optimal and efficient care.” - Alexander S. Misono, MD, MBA and colleagues.
- 2018: To become truly patient-centered, radiologists must move beyond traditional ‘business-as-usual’ report generation and find new ways to help patients access, comprehend, appraise, and apply the valuable information contained within our reports. Radiologists can and must do better.” – Nadja Kadom, MD and colleagues.
- 2018 RSNA Keynote: “We need to act like clinicians rather than image readers.” -Vijay Rao, MD (RSNA President)
Despite this call for change, a collaboration gap persists.
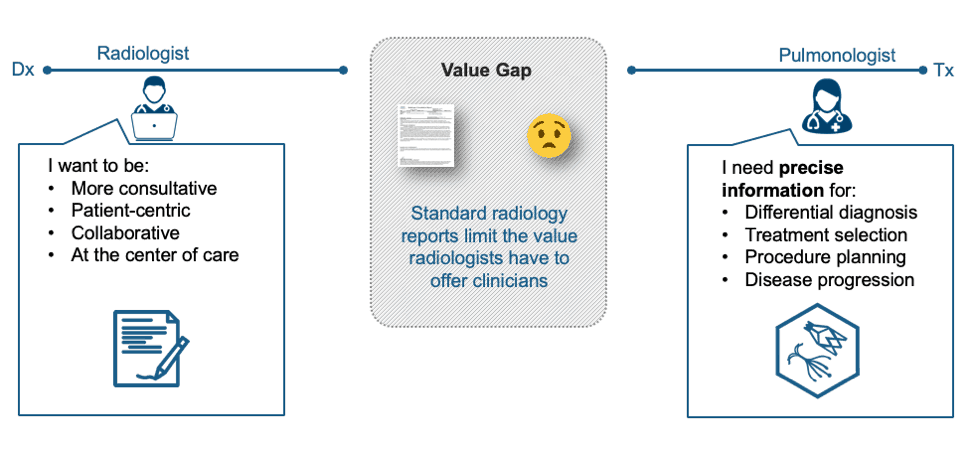
Collaboration Hurdles
While the desire to be more collaborative is growing stronger each year,
hurdles grow taller as well. Most
notably, productivity pressure on
radiologists continues to grow, leading to burnout (source). With pressure to read more cases, how can
radiologists take the extra time required to be more consultative, more
detailed, and more collaborative with clinicians?
Another barrier for radiologists—one that is more easily remedied—is simply knowing what high-value information clinicians need. For example, pulmonary valves were recently approved in the US market for the treatment of severe emphysema patients. A key exclusion criterion for these patients is the level of emphysema in each lobe and if heterogeneous to the upper lobes which can be determined through a quantitative CT (QCT) assessment, along with other key measures like fissure integrity as a measure of the presence or absence of collateral ventilation (source). Since fissure integrity assessment is not a routine part of a Chest CT read, a collaboration opportunity may be missed.
Fueling Collaboration through Precision Radiology
While radiology/clinician collaboration is certainly a multi-faceted issue without a silver bullet answer, we believe major strides can be made by equipping radiologists with precision radiology.
Our idea of precision radiology starts with quantitative image interpretation, allowing radiologists to report more objectively (e.g. “22% total high-density visually confirmed as ground glass and reticulations in the right and left lower lobes with moderate honeycombing pattern consistent with pulmonary fibrosis” vs. “presence of ground glass, reticulations and honeycombing consistent with pulmonary fibrosis”). By establishing a quantitative baseline scan, disease progression can be more objectively and precisely reported, allowing clinicians to make better informed care recommendations.
Radiology can once again situate itself at the center of patient care by embracing emerging technologies."
"AI will assist and augment radiologists. Ultimately, AI is going to help us make imaging faster and safer--and more quantitative, precise, and affordable."
Vijay Rao, MD., RSNA 2018 Keynote
We also think of precision radiology in terms of localized assessments at
the lobar or even sub-lobar (segmental) level.
“Precision therapy requires precision information” is a VIDA
mantra. For example, if emphysema is
concentrated within a particular sub-lobe, perhaps a therapy can target that
particular region rather than the entire lobe, preserving healthy tissue.
Precision radiology will eventually go beyond quantitative measurements
and highly localized analysis. Soon, with
the help of AI techniques, new biomarkers and models capable of predictive
analytics will emerge (example), further
advancing radiology’s collaborative potential at the center of care.
The
result of precision radiology is a “collaboration zone” where radiologists find
themselves delivering high value imaging insights to clinicians. Meanwhile, clinicians find themselves leveraging
their radiology departments more strategically as true clinical partners at the
center of care.
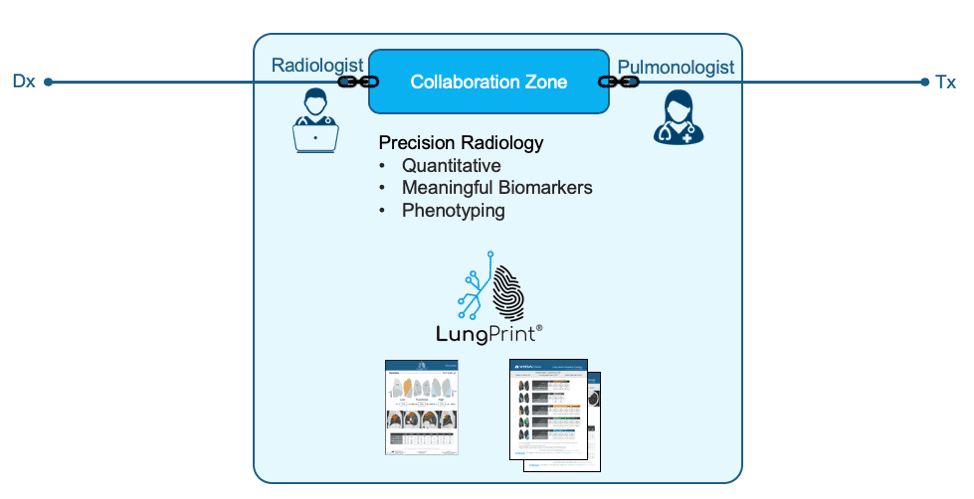
What about Efficiency?
With productivity pressures high, in order to fully realize the potential and opportunities of AI and quantitative analyses, companies like us must keep performance and efficiency at a high priority to successfully bridge the value gap; thus, empowering radiology to provide more valuable information to clinicians without impeding radiology’s efficiency. Precision radiology isn’t going to be embraced unless it can be deployed with a net neutral or better time impact. With this in mind, we have designed our LungPrint® analysis to automatically generate quantitative measures and to be integrated into the radiology workflow. Additionally, we’ve introduced novel visualizations intended on making chest CT interpretations faster. Early feedback shows that LungPrint will empower radiologists to provide more value and save radiologists’ time.
Conclusion
By empowering radiologists to efficiently deliver precision radiology—precise, quantitative, and clinically relevant—pulmonologists and other clinicians will find themselves in deeper and more frequent collaborations with radiologists. This richer collaboration among departments will benefit patients and providers through the use of highly precise, personalized care.
Cover image credit: miniara at pngtree.com (free vectors from pngtree.com)
-end-


